The discharge from Mountain Valley is not the end of the journey, but the beginning of a new chapter. For many residents and families, this transition can feel both exciting and unsettling. The structured environment that provided safety and support gives way to a less predictable daily life, where progress must be carried forward without the same immediate scaffolding.
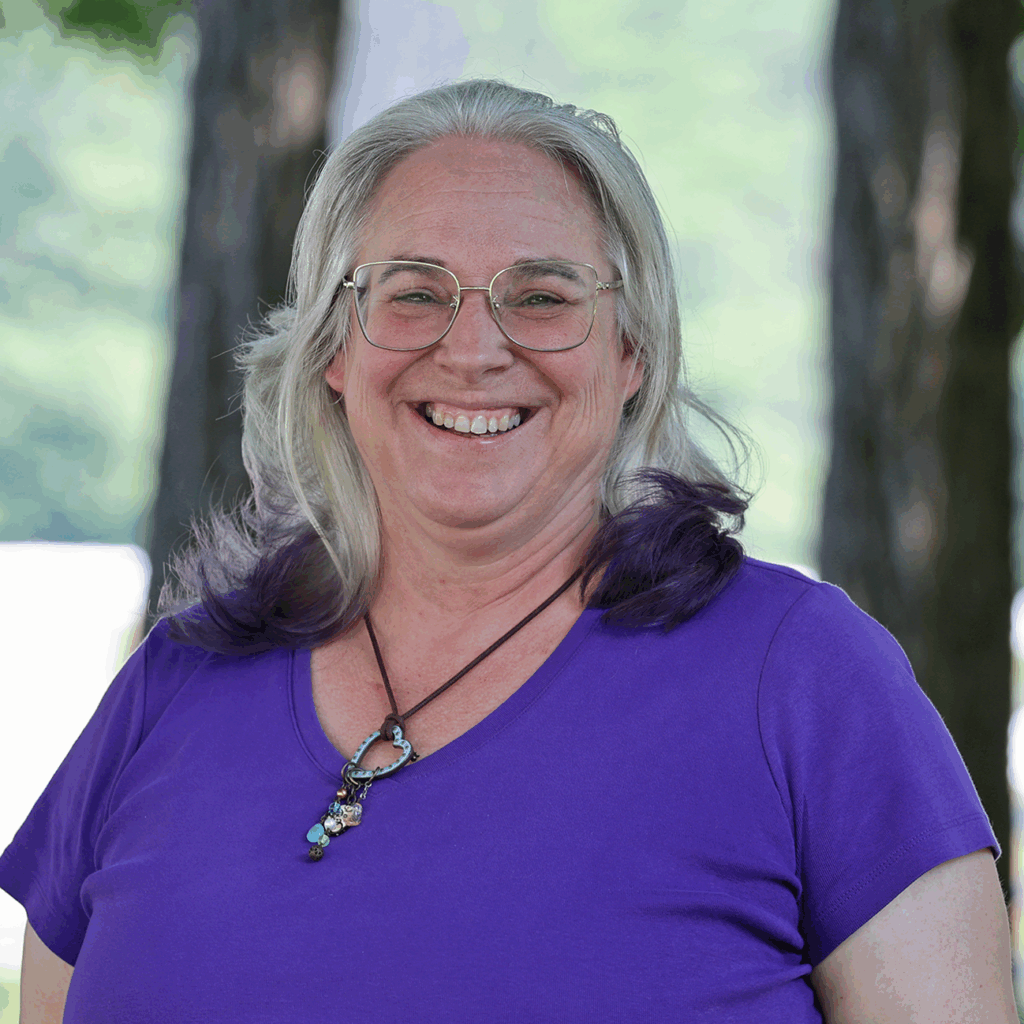
Phase 4: The Return was designed to bridge this gap. This optional, separately billed phase offers thirty days of structured guidance to help residents and families integrate what they have learned, establish lasting supports, and thoughtfully say goodbye to the community that has been central to their growth. Sharon McCallie-Steller, MS, MHC, who helped design Phase 4, has a long history with Mountain Valley and currently serves as the director of transition services. Learn more about Sharon’s background and Phase 4:
How did you end up at Mountain Valley?
I was in the middle of raising my family of four children, my youngest two were early teens getting through high school. I was starting to see the light at the end of the tunnel, and as my son was looking at colleges, I started doing some introspection myself about what I was really doing with my life.
Most of my career decisions had really been focused on making money and getting benefits. It wasn’t really about what I wanted, it was looking at what next job would give me the leg up that helps my family. At the time, that was an appropriate choice. But all of a sudden I was really questioning what I was doing.
One of my sons grew up with an anxiety disorder, and a lot of teachers and counselors helped us really learn how to help him. I was very participatory in all the school meetings, therapy, all the things. I started thinking about going back to graduate school, and when I was 40, I went back and got my mental health counseling degree. I looked for a job before I graduated because I have a family and I needed to get back to work.
I went to visit Mountain Valley and saw everything they did, and I felt like I was made for the job. I knew what it was like to be a parent of a child who struggled with anxiety. I was shocked they rolled the dice on me because I was a non-traditional applicant, in my mid-forties at the time, just getting out of school. I asked the clinical director at the time why he hired me, and he said, ‘you just can’t teach passion.’ I dove in and I learned so much, working as one of the first clinicians from 2014-2019, before Mountain Valley moved to Plainfield.
How did you land in your current role?
After Mountain Valley, I worked in an assessment program for boys in the foster care system, and as a therapist at a specialized boarding school. But that life was very intensive and COVID hit, so I started looking at other things. Will Laughlin ended up calling me and mentioned interest in transition work at Mountain Valley, adding some supports for families based on feedback he’d received. Will knew I had this experience, because I did a lot of family therapy and parent coaching as a clinician. He also knew I had the personal experience parenting a child with an anxiety disorder, and asked if I’d like to be part of the transition services team.
I think part of what has led me back to this moment is how can I help parents? Parenting is really hard, it’s hard in general. It dovetailed nicely, I was able to use my experiences and meld it all together to help support families post-treatment. I think a lot of times there’s a gap when someone leaves treatment and they start therapy outside of treatment. A new therapist doesn’t have the precise language of the sending program, and they don’t really know what’s gone in in the treatment center. Phase 4 helps with the continuity of care to have a bridge of someone who really understands ERP and knows how it all works. That’s an important part of what we’re doing with Phase 4 and our transition work.
Tell us a little more about how your background prepared you for this role?
I think my life experience helps me relate to parents. I have my own children, who are now from ages 24 to 36, and I’ve been through all stages of parenting. My son with anxiety struggled in so many ways, but he overcame his challenges and became a Marine. I have another son who has battled with addiction and is sober now. I’ve been through it. I’ve walked this path.
And I have a lot of experience in general. Before I went back to school, I worked in a lot of different industries doing all kinds of administrative work. That knowledge has really allowed me to be mindful of how to work with teams and succinctly put information together. Then work together to make sure we’re all moving in the same direction.
It’s kind of like I picked up all these pebbles on my way through life, now they’re in a jar and I’m using them in this work. It’s nice to feel that all the time I was doing other things, they were still valuable for what I’m doing today.
How did Phase 4 develop?
Our first round of transition services helped some families, but we found it didn’t help as many Mountain Valley families as we’d like. I wasn’t involved in the transition planning for families until the very end. We decided we should come at it from a different angle. We have three phases of treatment, and we want to do a fourth phase that’s a very specific, short-term support for families. A bridge from Mountain Valley to a more normalized environment that doesn’t have a robust therapeutic component. It might be home, it might be a boarding school, or maybe it’s college.
Zack and I got together and brainstormed on how to improve our transition process. We wanted Phase 4 to have the same type of approach as our other phases. We have a checklist, we have expectations of what we’re working on. But in this phase, it titrates down so we pull support back and guide families toward their community supports.
We decided I should come in to help with transition planning right from the start, and now I meet parents just a couple of weeks into their child’s treatment. I’m supporting the clinicians, making sure we’re having our meetings and that the right people are invited. It just takes another thing off their plate.
The clinician’s job is to work on treatment, and our parent coach Dr. Lisa Rosen’s job is to do the parent coaching so parents are learning about anxiety and OCD. And my job is to make sure all of us keep an eye on the clock. Because 90 days goes very quickly when you are steeped in treatment and visits.
I’m everyone’s executive functioning brain when it comes to transition planning, and it makes it an easier transition when I take on the parent coaching in Phase 4. Parents are already comfortable with me—they’ve seen me on meetings, and I often work on the family agreement with them as their child is leaving treatment.
It’s early, but how do you think Phase 4 is going so far?
I’m excited, we have two families we’re working with currently and a couple coming up. It’s already helping parents recognize their patterns as they show up—helping them problem solve and identify those patterns in their communication. It’s a nice way for parents to not feel like they’re alone in the wilderness for the first four weeks. They have someone they can call, and access to me after their child graduates. We’re finding that having these students work with a mentor they knew while in treatment helps to reduce barriers to communication. Our mentors are having consistent and meaningful communication with the students they’re working with.
We may find that families need support for longer than the 30 days we provide, and I can help them find the next step, like a parent coach for parents or an executive functioning coach for the student for example. I can also brainstorm with their educational consultant, if they have one, to help them get more support.
I host a post Mountain Valley parent support group every other week on Tuesdays. Parents can join anytime they want, and they can talk to other parents. That group has great advice and support for each other.
I’m really kind of steeped in it. Even if I don’t have the answers, I can offer that lifeline. It’s really rewarding to be that support for parents in a time where there’s so much going on.
What have you noticed has been most helpful for families during the transition?
A lot of my work is telling parents that they do know what they’re doing and helping them recognize old patterns. They do have the tools they need to succeed. I’m here to boost their confidence and be their cheerleader—you’ve got this, you really are moving forward. When you’re parenting a kid who struggles and has extra special needs, it’s hard to remember.