He who has overcome his fears will truly be free. -Aristotle
I woke up to a bright light and a loud roaring in my ears. I was hunched over, bouncing slightly in my seat. My face was pressed against something cold and hard. Where was I? How did I get here? I started to panic.
While I sat up and groped for my mind, for some clue to my situation, my chest began to heave like a sprinter and my normally sub-40 pulse banged out an urgent 200 BPM alarm in my head. I couldn’t form a thought and my body was clenched, holding on, trying not to fall any deeper into panic.
Even once I realized that I was on a 737 flying from San Francisco to Denver, I continued to grip my tray table as if it was the only thing keeping me from falling 30,000 feet to earth, or, worse, running down the center aisle screaming like a madman. For the rest of the flight I was absolutely gripped with fear, fear that I might spiral again into panic.
It wasn’t until much later that I was able to deconstruct the event, to connect the previous all-nighter in San Francisco and the two compensatory venti coffees slammed just before boarding to this very panic-worthy episode of falling asleep and waking up hyper caffeinated and completely disoriented. Now it all makes sense to me. At the time, though, and for many months later, the episode seemed random, out of the blue, and completely outside of my control. When, I wondered, might my mind and body betray me again.
***
Panic attacks are scary. They can also be self-perpetuating and invasive, insinuating themselves into new situations seemingly at random. Like the sumac we have here in New Hampshire, panic doesn’t always stay put once it takes root; it can send out secret subterranean tendrils which shoot up through the ground to claim random new territories.
Like sumac, the panic that started on that airplane began to generalize to other areas of my life: public speaking, overly formal business conversations, and even phone calls—anywhere I felt that a panic attack might have significant, if mostly social, consequences.
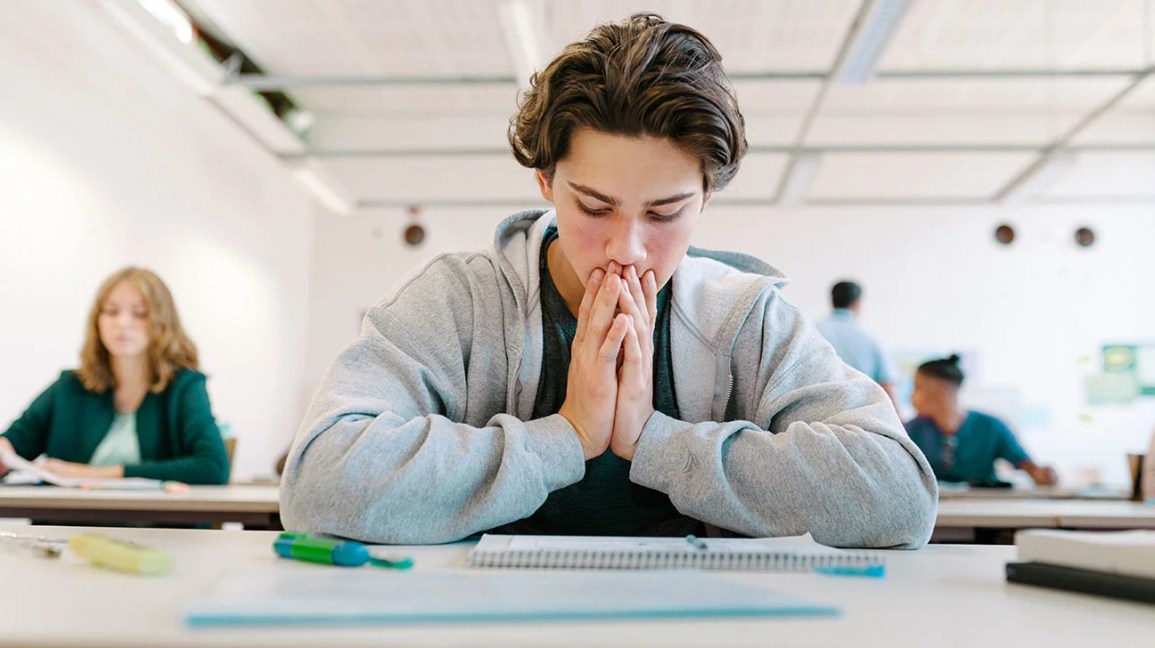
Panic entered my life, ironically, as I was approaching the pinnacle of my career as an elite adventure athlete. While I was calmly risking my life running hundreds of miles at a time in very dangerous places—the Sahara Desert, Taliban controlled parts of Tajikistan, -65°F arctic tundra—I was also developing a profound fear of airplanes, telephones, and everyday conversations. It did not make sense. My hard-won identity as a tough athlete—cool in the face of danger, a master of my own body and mind—was suddenly threatened by this outsized fear of everyday activities. So, who was I now? How might this unpredictable, episodic madness unravel my life and my career? I kept my struggles to myself, afraid that I might be losing my grip.
In order to remain employed and to continue my career as an athlete, I had to fly, I had to talk on the phone, I had to speak publicly. So I continued to muscle my way through these activities as best I could while trying, unsuccessfully, to manage the anxiety and stave off panic. My initial strategies included prescribed medication for public speaking or flying, breathing exercises, and—when possible—avoidance. None of these strategies worked. Some made things worse. Least helpful of all were my attempts to ignore or resist panicky feelings when they emerged. The more I fought those feelings, it seemed, the more they fought back and the stronger they became.
***
It wasn’t until months later that I bumbled into a concept that turned my white-knuckle experiences of flying and public speaking into something vaguely resembling actual exposure and response prevention therapy (ERP)—the clinical modality so successfully utilized by my colleagues at Mountain Valley Treatment Center. I was sitting on the floor of the Las Vegas International Airport failing to be hypnotized by a “fear of flying” hypnosis app I’d recently downloaded to my phone. Instead of dropping, as instructed, into a state of “deeeep relaxation” where the monotone hypnotist’s droll suggestions would insinuate themselves deep into my subconscious mind, I was wide awake, listening with my quite conscious mind, hoping this sleepy sounding guy would get to the freaking point before I had to board that damn airplane. Fortunately, he did.
As feelings of fear and panic approach, he suggested, invite them to come all the way to you. Lean into the feelings, experience them fully, consciously, and completely. Locate these sensations in your body, name them, feel them. Explore them with your mind the same way your tongue might explore the contours of a sore tooth. This guy was a nut, I thought. Invite panic? His approach makes no sense. So I decided to give it a try.
I boarded the plane, took my seat, and buckled my seatbelt. Right on cue, when the flight attendant started droning on about oxygen masks and exit lights and life preservers, the usual feelings of panic started to rise in me. But this time, instead of trying to push them back down, I invited them to join me, albeit a bit angrily. “Come on M#@$!* F#@!!!,” I mouthed silently, “bring it on! Let’s see what you’ve got. Okay, there you are, a tickle in my solar plexus, moving up my spine now. My head is filling with cotton and I’m getting dizzy. I’m handling this. Come on heart, you can beat faster than that. Is that all you’ve got? Bring it on!”
I wasn’t very nice to those feelings, but once I invited and engaged them, they proved less formidable than I’d thought. I did not fall from the sky. I did not run down the center aisle screaming like a madman. As I practiced this approach on subsequent flights and other high stress events, the feelings continued to show up, generally, when expected, but now they more or less moved along, they passed through me; I wasn’t there to block their path anymore. I stopped cursing my feelings and started engaging the feelings with calm, curious detachment.
As my sense of confidence and mastery over these feelings developed, it occurred to me that I had already been applying a similar mindset to other areas of my life for years. As an athlete, external challenges—a mountain, a race, a contest—elicited a sense of competition, of complete engagement, of “bring it on” defiance. But it had not occurred to me to apply that same mindset to “fear itself,” as Roosevelt put it, i.e. to an adversary that was fundamentally internal rather than external.
In the authoritative ERP training manual we use at Mountain Valley Treatment center, Exposure Therapy for Anxiety: Principles and Practice, by Brett J. Deacon and Jonathan S. Abramovitz, and Stephen P. H. Whiteside, this mindset is referred to literally as the “bring it on attitude.” During intentional exposures to highly distressing or triggering situations, the authors suggest that “instead of trying to resist or control unwanted or fearful emotions and experiences, patients should focus on better tolerating, accepting, and even welcoming these experiences…” This combination of exposure and full emotional engagement is at the core of exposure therapy. The “bring it on attitude” toward anxious feelings is the catalyst that activates exposures, making them therapeutic rather than simply unpleasant.
Once I recognized the connection between the challenges of adventure and the challenges of panic, my experience of anxiety actually began to shift from a threat to be avoided to an adventure to be engaged. A contest. Once I reframed them as adventures, my internal “anxiety expeditions” (what I now understand as “exposures”) became even more gratifying than my other expeditions, which were more dangerous but less scary. This, frankly, felt more badassed to me. When you successfully climb a mountain, it doesn’t make the mountain smaller. Instead, it makes you a mountaineer—freer to go where you want and to do what you want to do. That is the point of exposure therapy.
***
Several months ago, a very talented occupational therapist was considering a position at Mountain Valley. I knew that taking the position would move her from her high-level research and organizational work, back into the trenches of clinical care for highly anxious adolescents. It would be a huge change and a significant challenge, but her gift for clinical work was obvious and I hoped she would take the job. A few weeks after her initial interviews, I checked in with her.
“So, what are you thinking?” I asked.
“Well,” she answered, “honestly, I’ve been thinking a lot about it, Will. I’m just really nervous about the job.”
My heart sank. I understood her concerns but I was so disappointed. She would have been an incredible hire for Mountain Valley. While I tried to mask my disappointment and formulate a positive response, Kevi finished her thought.
“So I think I need to take the job.” In other words, bring it on!
For me, that interaction sums up the core of our philosophy at Mountain Valley: the evidence-based notion that engaging fear is the best way to flip it on its head, transforming anxiety from disability to ability, from enemy to ally. When our residents bravely engage in this work, as they routinely do, their personal Mount Everest of fear doesn’t necessarily get any smaller. Instead, they become mountaineers—confident and free to live the adventure they want.
Bring it on.
 As the external sensations of our world continue to become more abundant and all consuming, we often overlook the sensations of our inner world. One of the most important and foundational sensory systems we have is our interoceptive system. Interoception is our body’s internal radar of the condition of our body, conveying information about the state of what is happening within the bounds of our skin.
As the external sensations of our world continue to become more abundant and all consuming, we often overlook the sensations of our inner world. One of the most important and foundational sensory systems we have is our interoceptive system. Interoception is our body’s internal radar of the condition of our body, conveying information about the state of what is happening within the bounds of our skin.